IDENTIFYING A CONCUSSION
Myth. Professionals agree on the definition of a concussion.
Fact. Vague and inconsistent definitions create confusion and misunderstanding in sports-related concussion research. “The quagmire created by the use of inconsistent, overlapping and poorly defined terminology relating to brain injury research is exacerbated in sport-related research”.
Myth. A more accurate term for concussion is a head injury rather than a brain injury.
Fact. A more accurate term for a concussion is a brain injury rather than a head injury. In the athletic world, the terms concussion, mild traumatic brain injury (mTBI), mild closed head injury, and mild somatic brain injury are frequently utilized as synonyms. Since the mid-1990s, the use of the term mTBI, rather than mild closed head injury, has been encouraged by professionals and the Brain Injury Association of America, and is often used analogously with the term concussion.
Myth. The term mild concussion reflects the mild impact and effects of a concussion.
Fact. Because diffuse brain injury is assumed to occur when a person sustains a concussion, and no brain affliction should ever be considered minor, the use of the term mild brain injury is inaccurate. Johnson advocated for the use of the term subtle brain injury to describe a minor brain injury because the effects on the brain are difficult for the casual observer to recognize. Additionally, Kieslich reported that “minor head injuries can be a cause and cofactor in the etiology of stroke [in children]” . Given the possibility of death or significant brain damage resulting from an athlete sustaining another brain injury, the notion of a mild concussion is not supported.
Myth. The branch of medicine (epidemiology) which deals with causes, distribution, and control of concussions is always accurate and is easy to locate within the corresponding scientific literature.
Fact. Gathering accurate epidemiological information pertaining to concussions is a challenge due to variables such as: differing definitions for the term mild brain injury, a lack of documentation of its occurrence, under-reporting of injuries by physicians because a large percentage of athletes do not utilize healthcare providers when injured, and an under-reporting of injuries by the athlete.
Myth. Medical doctors are well trained in the area of concussions during medical school.
Fact. Sweeney cited studies reflecting “suboptimal sports medicine educational
experience” for residents and concluded that sports medicine received minimal focus in the United States when curricula were formulated. The research included a cited survey of 233 recently graduated chief residents that found that approximately 68% reported being less than comfortable managing a concussion sustained by an athlete. Hence, more thorough and accurate concussion education is needed for medical students, physicians-in-training, and physicians.
Myth. MRIs and CAT scans, neurocognitive/neuropsychological paper and pencil tests, and computer scoring tests are sensitive to all symptoms of a sported-related concussion (SRC).
Fact. Much of the current neurocognitive and neuroimaging instrumentation and many evaluation techniques are generally not sensitive enough in assessing and detecting all mild brain injury. This lack of sensitive instrumentation reveals the limitations of a scientific methodology that utilizes concrete, and thus observable, data as the only valid and reliable data for drawing conclusions. Brain injury research has historically focused attention more upon the cognitive dysfunctions than the physical and emotional dysfunctions that occur as the result of a concussion. Lezak noted that the disruptive effects of most brain lesions usually involve all three of these areas of brain functioning. Data need to be collected beyond cognitive consequences to more adequately evaluate all potential areas of dysfunction. Many contemporary neurocognitive approaches utilized for evaluating concussions have presented ongoing concerns. Reitan and Wolfson noted that typical medical assessment methods (i.e., neurology exam, EEG, and brain imaging techniques) utilized in determining adverse effects of mild brain injury are rather gross and insensitive and thus, false conclusions may be derived which report no neurological deficits were sustained.
Myth. Athletes are knowledgeable regarding the symptoms of a concussion.
Fact. Recent research concludes that athletes may not recognize concussion symptoms and, therefore, they may suffer unrecognized sports-related brain injury. This lack of symptom knowledge will interfere with the athletes’ ability to receive a timely healthcare assessment and corresponding appropriate medical care.
Myth. Male athletes and female athletes have the same chance of sustaining a concussion. Fact. A review of gender research suggests that female athletes are more prone to concussions than their male counterparts. Possible explanations for this are that female athletes are more open to report concussion symptoms as compared to their male counterpart and are more prone to sustaining an SRC than their male counterparts due to differences in anatomy and physiology.
Myth. Athletes will typically acknowledge when they have sustained a concussion.
Fact. Concussed athletes may not be cognitively capable of recognizing that they have sustained a concussion. They may not recognize all concussion symptoms and, therefore, may be unaware that they had incurred an SRC in the past. Additionally, SRC literature reveals that athletes tend to under-report mTBI injuries and that there is pressure to minimize sports injuries and play through the pain. Several reasons why an accurate perception of athletically related concussions is difficult to obtain include (a) athletes who sustain a concussion display an extensive number of symptoms from the obvious to the less obvious and subtle; (b) despite the numerous staff connected with athletics, including the team physician, limited knowledge in the area of concussion recognition is pervasive; (c) some players are hesitant to report personal symptoms to avoid medical suspension; and (d) some players minimize their injury because of their existing mindset to play hurt,.

CAUSES
Myth. An athlete needs to be hit on the head to sustain a concussion.
Fact. Because concussions can result from head [brain] trauma experienced via collisions, falls, or when a whiplash force is applied to the body, an athlete does not have to sustain a blow to the head for a concussion to occur. A recent study estimated that 1.6 million to 3.8 million concussions occur annually.
Myth. An athlete needs to be unconscious in order to sustain a concussion.
Fact. A concussion may or may not involve loss of consciousness. A common misperception exists regarding the need for unconsciousness to occur before a concussion diagnosis can be given. Approximately only 10% of concussions involve loss of consciousness.
Myth. Injury to the brain only occurs at the initial impact of the concussion.
Fact. Traumatic brain injury may be perceived as a process of initial and possible secondary events. Initial brain injury focuses on the injurious biomechanical force effects related to the impact, while secondary brain injury focuses on subsequent injurious neurochemical and neurometabolic changes occurring within the body that may exist for a significant period of time (i.e., weeks to months) after the initial impact.
Myth. The number of concussions or sub-concussive hits to the head are not important because each concussion and subconcussive hit is short-term and heals easily.
Fact. For most of the 20th century, the medical and sports community viewed a concussion as temporary and an entirely reversible physiological occurrence with no long term adverse effects. Since the 1940s, clinical research and postmortem evidence has existed for supporting the view that neuron damage occurs after a person sustains a concussion, and additionally, repeated “minor injury,” such as a concussion and a subconcussive hit, could result in progressive and cumulative permanent neuron loss and corresponding structural damage to the brain. More recently, concern has been voiced regarding the adverse cumulative effects of subconcussive hits to the head. The estimated number of subconcussive hits to the head occurring during a professional football season is 900 to 1,500 (Allen, 2010). Unfortunately, common football slang such as “ding” and “had his bell rung” reflect perceptions that reinforce the false notion that concussions are not serious.
EFFECTS
Myth. There is no relationship between concussions and the later occurrence of depression and neurologic diseases.
Fact. Prior traumatic brain injury has been linked to depression, Parkinson’s, Alzheimer’s, and chronic traumatic encephalophy (CTE). CTE is a degenerative disease that affects the brain and is believed to be caused by repeated head trauma (concussions and subconcussive hits to the head) resulting in large accumulations of proteins that kill cells in regions responsible for mood, emotions, and executive functioning.
Myth. Concussion symptoms do not overlap with symptoms of attention deficit hyperactivity disorder.
Fact. When individuals are suffering from attention, memory, or other information processing deficits, TBI or mTBI should be considered as possible diagnoses, since these symptoms are all marked manifestations of TBI. Some children and adolescents who had been diagnosed with an attention deficit hyperactivity disorder were found to be displaying symptoms of acquired traumatic brain injury upon receiving a more comprehensive assessment.
Myth. Concussion symptoms are not similar to the symptoms experienced by persons who are under the influence of alcohol.
Fact. Concussion symptoms mimic numerous symptoms experienced by a person who has ingested too much alcohol. These symptoms include, but are not limited to, slurred speech, short-term and long-term memory deficits, fatigue, hand–eye coordination delays, personality changes, mood swings, gross motor coordination delays, headaches, dizziness, and sleep problems.
Myth. Sports-related concussion impacts cannot be compared to motor vehicle accident impacts.
Fact. Documentation exists within sports research that SRC impacts are comparable to motor vehicle accident-related concussion impacts. For example, the impact speed of a professional boxer’s punches have been measured at 20 mph and the impact speed of a football player’s tackle on a stationary player at 25 mph. A soccer ball’s impact speed has been measured at 70 mph.

MANAGEMENT
Myth. After sustaining a concussion, return to play (RTP) standards employ objective, evidence based standards that drive multidisciplinary treatment.
Fact. “The science of concussion is at early stages, and therefore, management and return to play decisions remain largely in the realm of clinical judgment on an individualized basis”. Various authors have raised concern that expert opinion and related clinical judgments may be subject to conflicts of interest. It is imperative, therefore, that accurate, unbiased, and in-depth knowledge of SRCs and related management approaches be gathered from a multidisciplinary team of healthcare professionals who are adequately trained and free from conflicts of interest.
Myth. It is physically safe and healthy for an athlete to RTP after sustaining a concussion even if he or she is still experiencing minor concussion symptoms.
Fact. Sports medicine experts agree that an athlete should not be able to participate in contact sport competition while still experiencing any symptoms of a concussion. Furthermore, these experts concur that athletes should not RTP until concussion symptoms are no longer being experienced both at rest and during physical exertion. More recently, the original concept of rest has been expanded from physical rest to include cognitive rest. The concept of rest should be expanded to include the concept of emotional rest. Emotional rest includes providing the injured athlete with a relaxing and stress free environment during the functional recovery process. It is imperative that the brain adequately rests in all areas in order to heal. Brain rest involves the limiting of emotional,
physical, and cognitive activities. Overloading the brain is, in effect, causing the brain to short circuit. Additional brain injuries may occur as the result of sustaining another concussion after returning to play too early in the functional recovery process. The detrimental effect of the second concussion, referred to as second impact syndrome, places the athlete at further risk of significant brain damage that could result in permanent disability and, in rare instances, death.
Myth. A student-athlete can safely and productively return to the classroom even though he or she is experiencing symptoms related to a concussion.
Fact. Individualized treatment should be employed for student-athletes demonstrating cognitive deficits and emotional and physical needs upon returning to the classroom following a concussion. An interdisciplinary approach should be utilized to design a plan for the returning student’s education. Appropriate educational accommodations and modifications of the classroom setting should be considered. Because fatigue is a common and significant symptom, some suggested accommodations are frequent breaks (i.e., 5 minutes every half hour within a quiet area of the building), a reduced or modified school day and or school week, and provision for a place that offers quiet time. In addition, caution should be employed when encouraging an injured student-athlete to complete school-related tasks during the late afternoon and evening hours since a person with a concussion may become fatigued as the day progresses. It is essential for recovery to provide the student with a serene home environment for enabling cognitive, emotional, and physical rest.
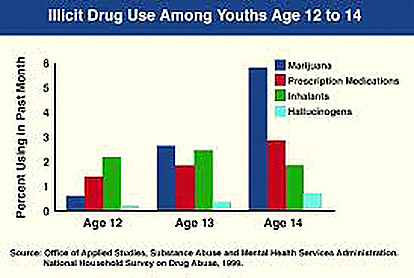
Myth. It is safe to drink alcoholic beverages and use street drugs while functionally recovering from a concussion.
Fact. An athlete should refrain from the use of alcohol while recovering from a concussion because alcohol use may impede the healing process. Furthermore, substance use should be avoided because greater adverse brain changes have been found to occur in brains of patients who experienced both TBI and substance abuse than in patients who experienced only one of these two issues.
SOCIAL IMPLICATIONS AND POLICY
Myth. A concussion only affects the individual who sustained it.
Fact. A concussion affects not only the individual who sustained it but also others who are close to the concussed individual. Numerous adverse implications of TBI on the family include risk of suicide, divorce, chronic unemployment, economic stress due to lost earnings, and substance abuse. The family system becomes further impacted as its members also report depression, social isolation, anger, and overall disruption of family relationships.































































 One third of all high school students will receive a concussion during their four years of school.
One third of all high school students will receive a concussion during their four years of school.  People with PCS seek brain stimulation and/or self-medication to counteract the pain of anxiety and depression.
People with PCS seek brain stimulation and/or self-medication to counteract the pain of anxiety and depression.  Two million adolescents attempt suicide each year.
Two million adolescents attempt suicide each year.





